Concise Summary
Digestive disorders like IBS, IBD, and other gastrointestinal conditions affect millions of Americans, causing chronic pain, bloating, and lifestyle disruption. Understanding prevalence, symptoms, risk factors, and treatment options is essential. This article explores how these disorders impact the U.S. population, evidence-based management strategies, emerging therapies, and lifestyle approaches to support digestive wellness and improve quality of life.
Introduction: Digestive Disorders in the U.S.
Digestive disorders are among the most common chronic conditions in the U.S., affecting over 70 million Americans annually (NIH, 2023). Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two primary categories, but the spectrum also includes celiac disease, gastroesophageal reflux disease (GERD), and functional dyspepsia.
Symptoms can vary from mild discomfort to severe pain, diarrhea, constipation, and fatigue. The burden is not only physical but emotional, often affecting work performance, social life, and mental well-being.
Real-life Example: A 34-year-old New Yorker with IBS struggled with unpredictable symptoms for years, affecting her career and social life. After working with a gastroenterologist and adopting a personalized diet, she experienced significant symptom relief and improved daily functioning.
Understanding IBS, IBD, and Related Disorders
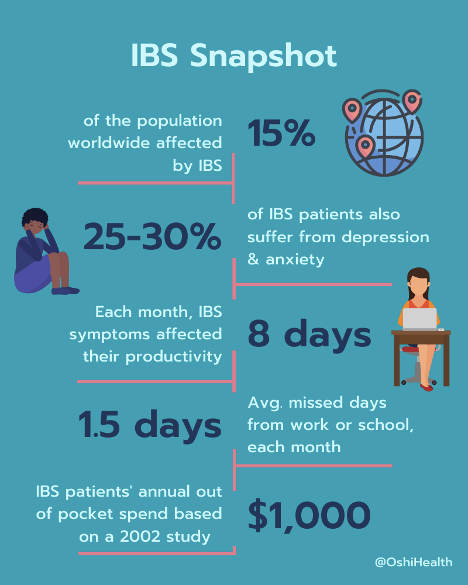
1. Irritable Bowel Syndrome (IBS)
- Definition: A functional GI disorder characterized by abdominal pain, bloating, and altered bowel habits (diarrhea, constipation, or both).
- Prevalence: Affects 10–15% of Americans.
- Triggers: Stress, dietary factors, hormonal changes, and gut microbiome imbalance.
Example: A software engineer in San Francisco found that stress at work triggered IBS flare-ups, alleviated through mindfulness practices and dietary adjustments.
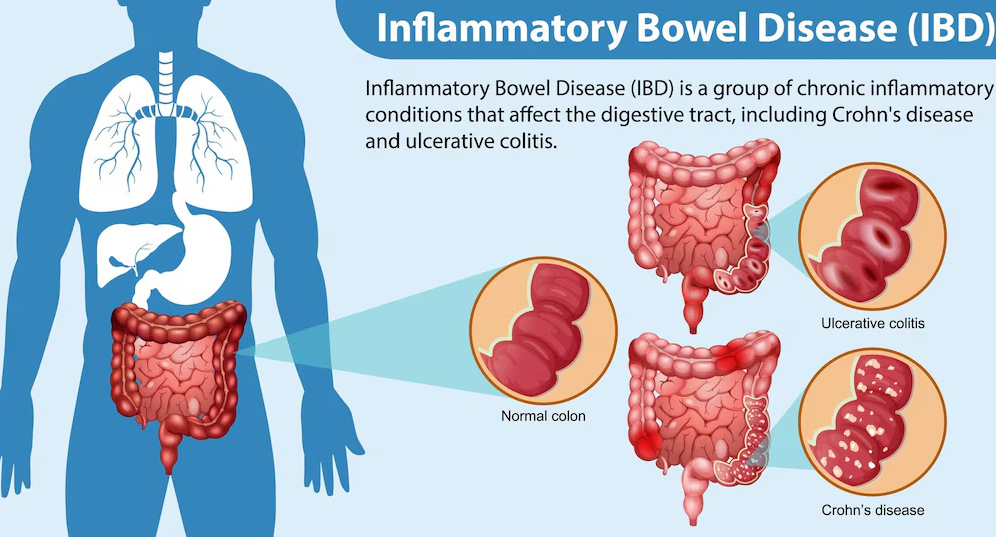
2. Inflammatory Bowel Disease (IBD)
- Definition: Chronic inflammatory conditions, including Crohn’s disease and ulcerative colitis, that damage the intestinal lining.
- Prevalence: Approximately 3 million Americans have IBD.
- Symptoms: Abdominal pain, diarrhea, rectal bleeding, fatigue, and weight loss.
Example: A college student with Crohn’s disease in Chicago uses biologic therapy and a structured diet plan to manage inflammation and maintain academic performance.
3. Other Common Digestive Disorders
- GERD: Chronic acid reflux causing heartburn and esophageal irritation; affects 20% of U.S. adults.
- Celiac Disease: Autoimmune reaction to gluten; prevalence of 1% of Americans, often underdiagnosed.
- Functional Dyspepsia: Upper abdominal discomfort with no apparent structural cause; impacts ~11–15% of U.S. adults.
Causes and Risk Factors
- Genetics: Family history increases susceptibility, especially for IBD and celiac disease.
- Diet: High-fat, low-fiber diets can exacerbate IBS; gluten triggers celiac flare-ups.
- Stress and Lifestyle: Chronic stress worsens symptoms via the gut-brain axis.
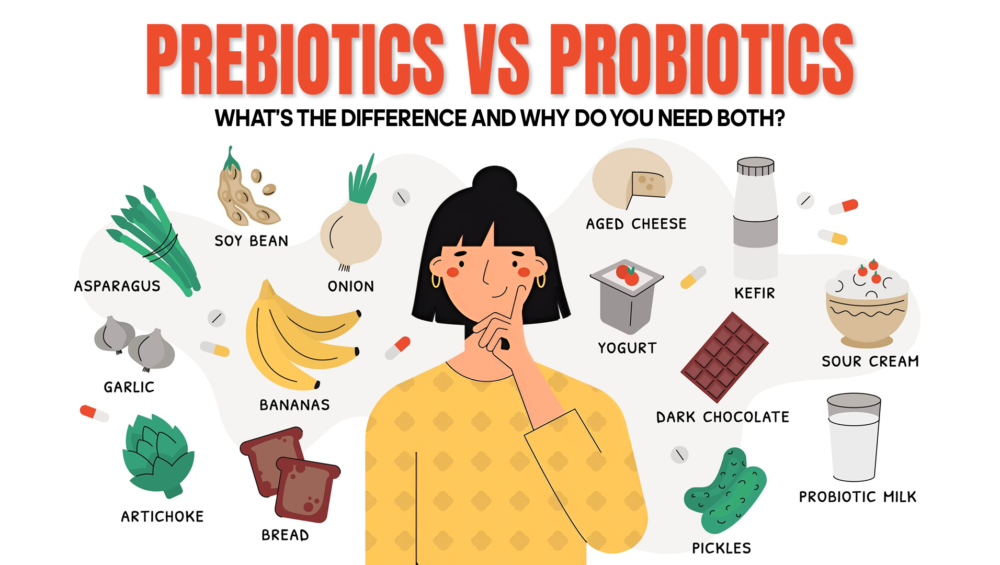
- Microbiome Imbalance: Disrupted gut bacteria contribute to IBS, IBD, and food intolerances.
- Medications: Long-term NSAID use or antibiotics may irritate the GI tract.
Signs and Symptoms to Watch For
- Persistent abdominal pain or cramping
- Bloating or gas
- Chronic diarrhea or constipation
- Rectal bleeding or black stools
- Unexplained weight loss or fatigue
Tip: Early recognition of red-flag symptoms is crucial for timely intervention and preventing complications.
Management and Treatment Approaches
1. Dietary Interventions
- Low FODMAP Diet: Reduces fermentable carbohydrates that trigger IBS symptoms.
- Anti-inflammatory Foods: Omega-3 rich foods, turmeric, and antioxidants help manage IBD inflammation.
- Gluten-Free Diet: Essential for celiac patients.
- Hydration & Fiber: Soluble fiber improves bowel regularity in IBS and functional dyspepsia.
Example: A Florida-based nurse adopted a low-FODMAP diet and probiotics to reduce bloating and irregular bowel habits, seeing measurable improvement within weeks.
2. Medications
- IBS: Antispasmodics, laxatives, or anti-diarrheal agents depending on symptom type.
- IBD: Biologics, corticosteroids, and immunomodulators reduce intestinal inflammation.
- GERD: Proton pump inhibitors (PPIs) or H2 blockers manage acid reflux.
Tip: Medications are most effective when combined with dietary and lifestyle strategies.
3. Lifestyle Modifications
- Stress Reduction: Yoga, meditation, and cognitive behavioral therapy (CBT) reduce IBS flares.
- Regular Exercise: Improves bowel motility and reduces inflammation.
- Sleep Hygiene: Adequate rest supports gut repair and immune function.
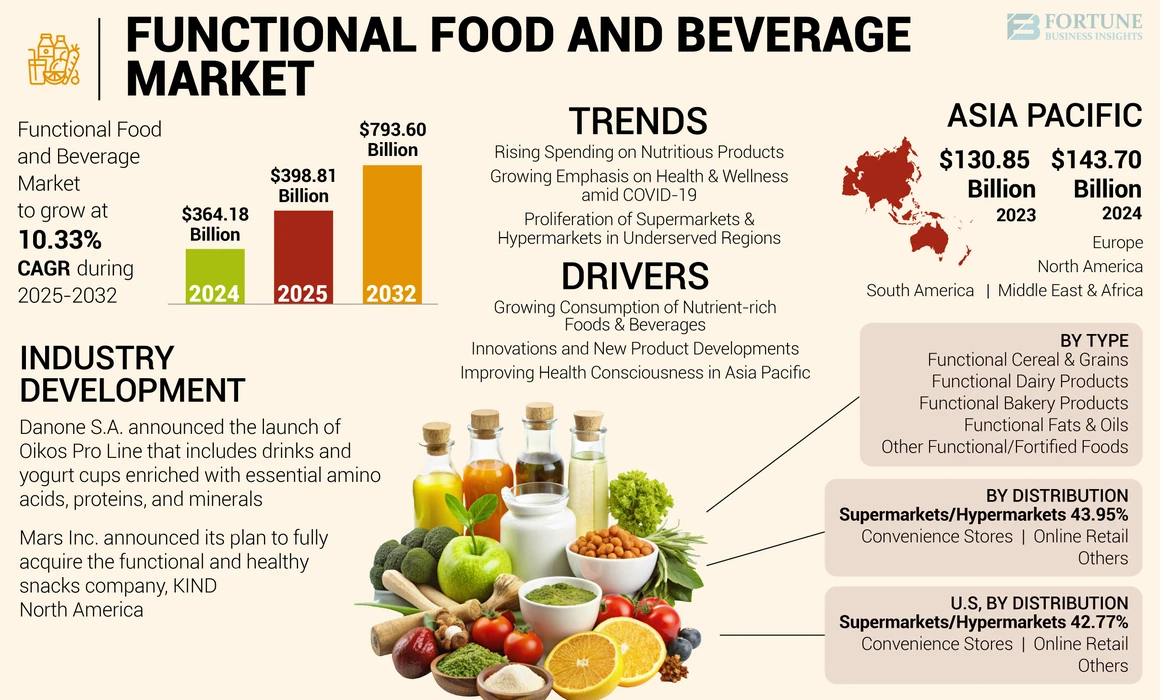
4. Emerging Therapies
- Microbiome-Based Treatments: Fecal microbiota transplantation (FMT) and precision probiotics show promise for IBS and IBD management.
- Personalized Nutrition Apps: AI-driven tools help Americans track diet, symptoms, and microbiome health.
- Integrative Approaches: Combining herbal remedies, probiotics, and functional foods with conventional care.
FAQs
1. How common is IBS in the U.S.?
IBS affects roughly 10–15% of Americans, making it one of the most prevalent functional gastrointestinal disorders. Symptoms often appear in early adulthood, with women more frequently affected. Early diagnosis, stress management, and dietary interventions can significantly improve quality of life.
2. What is the difference between IBS and IBD?
IBS is a functional disorder with no structural damage, while IBD (Crohn’s and ulcerative colitis) causes chronic inflammation and tissue injury. IBS symptoms include pain, bloating, and altered bowel habits; IBD may involve bleeding, weight loss, and systemic inflammation.
3. Are digestive disorders hereditary?
Genetics play a role, particularly in IBD and celiac disease. Family history increases risk, but lifestyle, diet, and microbiome composition also significantly influence disease onset and severity.
4. Can diet alone manage IBS?
Dietary interventions like low-FODMAP diets, soluble fiber, and anti-inflammatory foods can reduce symptoms for many, but some patients require medications or stress management for optimal results.
5. What are the treatment options for IBD?
IBD treatment includes biologics, corticosteroids, immunomodulators, dietary adjustments, and sometimes surgery. Ongoing monitoring and collaboration with gastroenterologists are essential to prevent complications and maintain remission.
6. How does stress affect digestive disorders?
Stress activates the gut-brain axis, altering motility, increasing pain perception, and triggering flare-ups in IBS and IBD. Mindfulness practices, therapy, and exercise are critical for symptom management.
7. Are probiotics beneficial for IBS and IBD?
Probiotics can help restore gut flora balance, reduce bloating, and improve bowel regularity in IBS. Certain strains may also complement IBD treatment, though evidence is stronger for IBS than IBD.
8. When should I see a doctor for digestive issues?
Consult a gastroenterologist if you experience persistent abdominal pain, bleeding, unexplained weight loss, chronic diarrhea, or constipation lasting more than a few weeks. Early evaluation prevents complications.
9. Can lifestyle changes make a real difference?
Yes. Adequate sleep, stress reduction, regular exercise, and mindful eating improve gut motility, reduce inflammation, and enhance quality of life for Americans with digestive disorders.
10. Are there natural remedies that help with digestive health?
Herbs like ginger, peppermint, chamomile, and turmeric, combined with fermented foods and prebiotic fibers, can complement conventional treatment by reducing inflammation and supporting microbiome balance.
Key Takeaways for Americans
- Digestive disorders like IBS and IBD are prevalent and impact millions of U.S. residents.
- Early recognition, medical guidance, and lifestyle adjustments are crucial.
- Combining dietary interventions, stress management, and medications leads to better outcomes.
- Emerging microbiome-based therapies and integrative approaches offer hope for personalized digestive care.
Conclusion: Improving Digestive Health Across the U.S.
IBS, IBD, and other digestive disorders present complex challenges for Americans, affecting both physical and emotional well-being. Through a combination of diet, lifestyle, medications, and emerging therapies, individuals can manage symptoms effectively and improve their quality of life. Public awareness, early diagnosis, and evidence-based interventions are essential for creating a healthier population.
Read this also : https://myhealthhacks.us/emerging-technologies-in-gut-microbiome-research-transforming-digestive-health-in-the-u-s/