Summary
The U.S. is battling a growing lifestyle disease epidemic fueled by obesity, diabetes, and cardiovascular conditions. Rising healthcare costs, reduced productivity, and declining life expectancy highlight the urgency of preventive action. With digital health innovations, public policy shifts, and cultural changes, America has a chance to reverse this trend. This article explores whether the U.S. can realistically curb lifestyle diseases and what the future holds.
Introduction: Why the Future of U.S. Health Depends on Lifestyle Choices
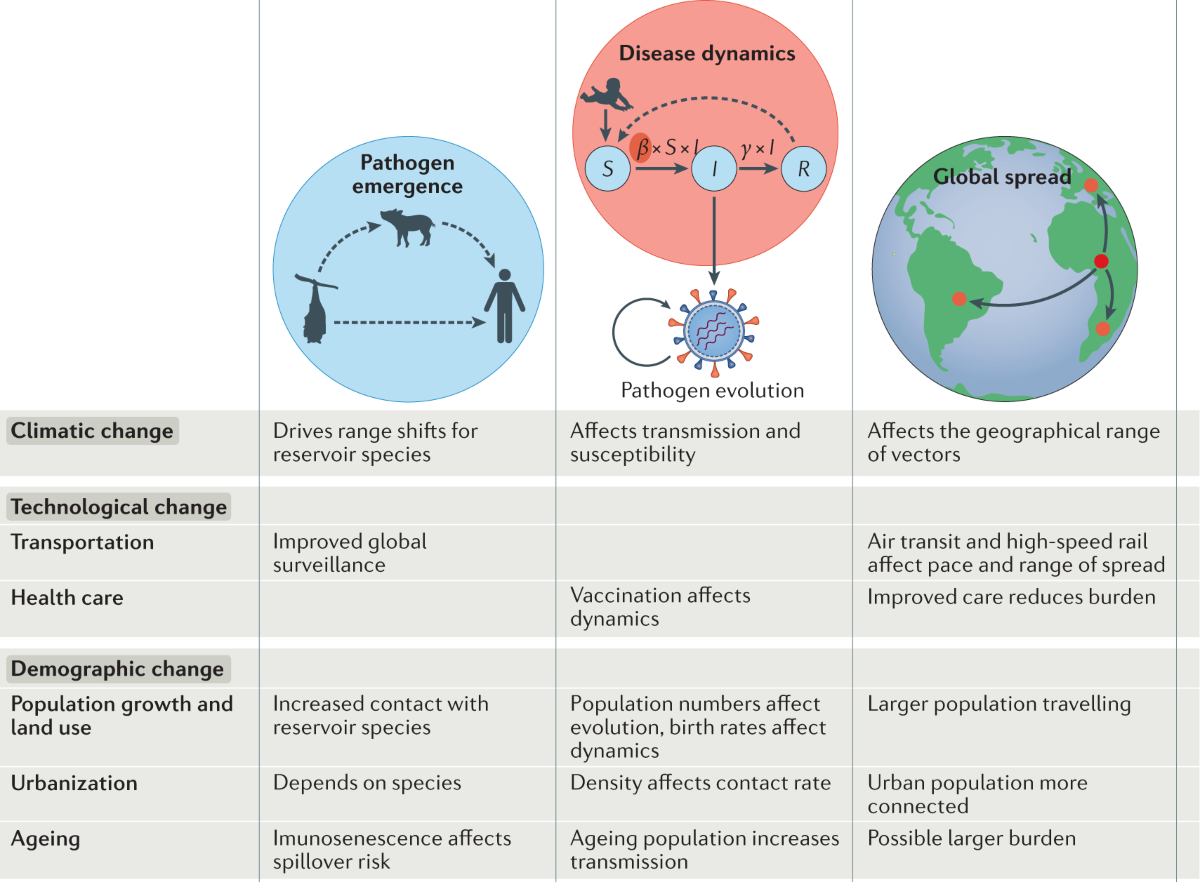
America is standing at a health crossroads. For decades, advances in medicine helped reduce deaths from infectious diseases and extended life expectancy. But today, the nation faces a new enemy—lifestyle diseases. Unlike infections caused by viruses or bacteria, lifestyle diseases are often the result of poor diet, lack of exercise, stress, and unhealthy habits.
According to the Centers for Disease Control and Prevention (CDC), 6 in 10 American adults live with at least one chronic disease, and 4 in 10 live with two or more. These conditions—obesity, diabetes, hypertension, cardiovascular disease—are preventable, yet they are the leading causes of death and disability in the United States.
The rise of these diseases has wide-reaching consequences. Healthcare costs are ballooning, productivity is declining, and American life expectancy has begun to stagnate. The question is no longer whether lifestyle diseases are a problem—it’s whether the U.S. has the willpower, resources, and policies to stop this epidemic before it spirals further out of control.
What Are Lifestyle Diseases and Why Do They Matter for America’s Future?
Lifestyle diseases are non-communicable diseases (NCDs) closely linked to individual habits and behaviors. These include:
- Obesity
- Type 2 Diabetes
- Hypertension (High Blood Pressure)
- Cardiovascular Disease
- Certain Cancers
- Chronic Respiratory Conditions
The reason they matter so much for America’s future is twofold:
- They are preventable. Most lifestyle diseases can be reduced or delayed with healthier habits.
- They affect national strength. These diseases reduce workforce productivity, increase healthcare spending, and even weaken military readiness.
Real-life example: Consider a 45-year-old American office worker struggling with obesity, fatigue, and rising healthcare costs. His employer sees lower productivity, his family faces emotional strain, and the healthcare system shoulders long-term costs. Multiply this by millions of people nationwide, and you see why lifestyle diseases are called a silent epidemic.
How Big Is the Lifestyle Disease Epidemic in the U.S.?
The numbers are sobering.
- Obesity: As of 2023, about 42% of American adults are classified as obese. Researchers project this number could climb to 50% by 2030 if current trends persist.
- Diabetes: Roughly 1 in 10 Americans has diabetes, with most cases being Type 2, directly tied to diet and lifestyle.
- Cardiovascular Disease: Responsible for 1 in every 5 deaths, heart disease remains the leading cause of mortality in the U.S.
- Healthcare Costs: The U.S. spends over $4.1 trillion annually on healthcare, and chronic diseases account for the majority of that spending.
There are also geographic disparities. Southern states like Mississippi and Alabama report obesity rates above 40%, while states like Colorado and Hawaii remain below 30%. These differences often reflect access to healthy foods, safe environments for exercise, and education levels.
If trends continue unchecked, the U.S. could face a public health crisis rivaling any pandemic—but one that unfolds slowly over decades instead of suddenly.
Key Drivers Behind the Epidemic
To understand the future, we must first examine what’s driving the present epidemic:
- Dietary Shifts: Fast food, processed snacks, and sugary drinks dominate the American diet. The rise of convenience eating has come at the cost of nutritional value.
- Sedentary Lifestyles: With remote work, digital entertainment, and long commutes, Americans spend more time sitting than ever before. Physical inactivity is now considered a leading risk factor for premature death.
- Mental Health Stressors: Chronic stress, anxiety, and sleep deprivation all worsen physical health. Stress eating and lack of rest are directly linked to weight gain and cardiovascular risk.
- Socioeconomic Inequalities: Millions of Americans live in food deserts, areas where affordable, healthy food is scarce. Similarly, many lack safe spaces to exercise.
- Marketing & Policy Gaps: While tobacco and alcohol advertising face strict regulation, junk food marketing remains aggressive, especially targeting children.
Can Preventive Healthcare Be America’s Game-Changer?
One of the most promising solutions is shifting from treatment-focused healthcare to prevention-first healthcare.
Why Preventive Care Matters:
- Preventive screenings can detect diabetes, hypertension, and cancers early, improving survival rates.
- Wellness programs reduce absenteeism and boost productivity.
- Preventive investments reduce long-term costs.
Real-Life Example:
Google provides on-campus gyms, wellness coaches, and healthy meals to its employees. These initiatives reduce healthcare claims and improve employee retention—showing that prevention pays off for both individuals and organizations.
Employer-driven wellness could include:
- Subsidized gym memberships.
- Access to health coaching apps.
- Incentives for achieving step or nutrition goals.
By normalizing preventive care, the U.S. can address the disease before it reaches a crisis stage.
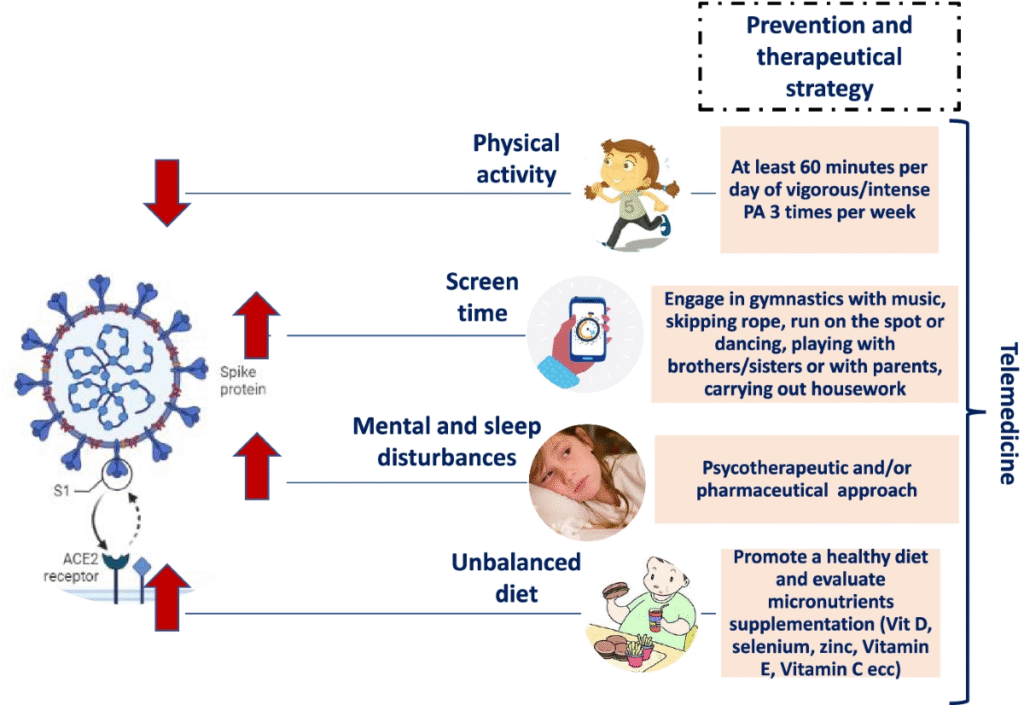
The Role of Technology and Digital Health in Curbing Lifestyle Diseases
Technology is rapidly changing the way Americans manage health.
- Telemedicine: Expands access to preventive care, especially in rural areas where doctor shortages are common.
- AI-based health apps: Predict risks based on data inputs and recommend interventions.
- Wearable devices: Apple Watch, Fitbit, WHOOP, and continuous glucose monitors provide real-time insights into activity, heart rate, and blood sugar.
- Gamification: Fitness apps like Strava or Peloton motivate users through challenges and community engagement.
Example: A diabetic patient using a continuous glucose monitor can instantly see how a particular meal affects blood sugar. This level of real-time feedback encourages healthier eating decisions, which traditional healthcare visits cannot provide.
Public Policy: What Steps Can the Government Take?
Policy is a powerful driver of health outcomes.
Potential actions include:
- Taxation on sugary drinks: Similar to cigarette taxes, soda taxes can reduce consumption. Philadelphia implemented such a tax in 2017, leading to a 38% drop in sugary drink sales.
- Subsidies for healthy food: Lowering prices for fruits and vegetables makes them more accessible.
- Mandatory food labeling: Clearer front-of-package labels to help consumers make informed decisions.
- Advertising restrictions: Limiting junk food ads aimed at children.
- Medicare/Medicaid incentives: Rewarding preventive care participation.
Community and Cultural Shifts: Is the U.S. Ready?
Ultimately, healthcare solutions won’t succeed unless cultural shifts accompany them.
- Local wellness programs: Farmers’ markets, bike lanes, and community fitness centers encourage healthier lifestyles.
- Prevention-first mindset: Moving away from the idea that “medicine fixes all problems” toward “lifestyle prevents most problems.”
- Blue Zones lessons: Areas in the world where people live longer (like Okinawa, Japan) focus on diet, community, and low-stress living. Some U.S. communities have adopted these principles with measurable success.
Economic Impact: What’s at Stake if We Fail?
The financial consequences of ignoring lifestyle diseases are staggering.
- $4.1 trillion annually is spent on chronic diseases in the U.S.
- Rising insurance premiums (6–8% annually) burden both individuals and employers.
- Reduced workforce productivity—employees miss work or underperform due to illness.
- National security concerns: 1 in 3 young Americans is unfit for military service due to obesity.
Without intervention, lifestyle diseases could become the single greatest threat to American economic stability.
Future Outlook: Can the U.S. Realistically Reverse This Epidemic?
Optimistic Scenario:
- Digital health tools become mainstream.
- Preventive care gains policy support.
- Cultural emphasis shifts toward wellness.
- By 2040, obesity rates stabilize, and chronic disease prevalence decreases.
Pessimistic Scenario:
- Continued fast-food consumption and sedentary lifestyles.
- Healthcare spending rises unsustainably.
- Life expectancy declines further.
Lessons from Abroad:
- Japan: National “Metabo Law” requires companies to measure employees’ waistlines and provide counseling for overweight workers.
- Nordic countries: Strong emphasis on outdoor activity, social welfare, and balanced diets reduce lifestyle disease prevalence.
For the U.S., the future depends on multi-stakeholder collaboration between individuals, healthcare providers, employers, and policymakers.
Practical Takeaways: What Americans Can Do Now
Individuals:
- Aim for 150 minutes of physical activity weekly.
- Adopt a balanced diet rich in whole foods.
- Prioritize 7–9 hours of sleep nightly.
- Reduce alcohol and tobacco use.
Families & Communities:
- Share home-cooked meals.
- Encourage group exercise or walking clubs.
- Advocate for healthier school lunches.
Employers:
- Offer wellness incentives.
- Create flexible schedules that support work-life balance.
Policy Advocates:
- Support local wellness initiatives.
- Push for stronger preventive care coverage.
Trending FAQs
1. What are the main causes of lifestyle diseases in the U.S.?
The primary causes of lifestyle diseases in the United States are poor nutrition, lack of regular physical activity, chronic stress, smoking, and excessive alcohol consumption. Modern conveniences such as fast food, desk jobs, and screen-heavy lifestyles have created a perfect storm for health decline. Socioeconomic factors, like limited access to affordable healthy foods and healthcare, also play a significant role in why certain populations are more affected than others.
2. Can technology really reduce obesity and diabetes?
Yes, technology has the potential to dramatically reduce obesity and diabetes rates. Wearables like Fitbit and Apple Watch track daily activity, heart rate, and calories burned, creating real-time accountability. Continuous glucose monitors give diabetics actionable insights into how specific foods affect their blood sugar. Telemedicine and AI-based coaching apps also make it easier for patients to access medical advice, nutrition plans, and fitness support. These tools empower individuals to make healthier choices consistently, bridging the gap between intention and action.
3. How much does the U.S. spend on lifestyle diseases annually?
The U.S. spends more than $4.1 trillion every year on healthcare, and the majority of that spending is tied to chronic, lifestyle-related diseases such as obesity, diabetes, and heart disease. These costs are not just medical bills—employers also suffer from productivity losses, absenteeism, and early retirements. If lifestyle diseases remain unchecked, healthcare spending will continue to rise unsustainably, potentially crowding out other vital areas like education and infrastructure. Preventive care and wellness initiatives can significantly reduce this burden over time.
4. Are preventive healthcare programs effective in America?
Yes, preventive healthcare programs can be highly effective, but their success depends on participation rates and long-term engagement. Programs offering regular health screenings, workplace wellness initiatives, and lifestyle coaching have proven to reduce rates of hypertension, diabetes, and obesity. For example, companies like Johnson & Johnson saved millions in healthcare costs by investing in employee wellness. However, many Americans still prioritize treatment over prevention, so building awareness and incentives is critical for success.
5. What role does diet play in lifestyle disease prevention?
Diet plays a central role in preventing lifestyle diseases because what we eat directly affects our weight, blood sugar, cholesterol, and heart health. A diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can reduce the risk of obesity, diabetes, and cardiovascular disease. Conversely, diets high in processed foods, sugar, and saturated fats dramatically increase health risks. Research consistently shows that even small dietary changes, such as reducing sugary drinks or eating more fiber, can have lifelong positive impacts.
6. How do Blue Zones provide a model for U.S. health?
Blue Zones—regions of the world where people live longer, healthier lives—offer a powerful model for addressing lifestyle diseases in America. Communities in Okinawa (Japan) and Sardinia (Italy) emphasize plant-based diets, strong social networks, active daily living, and stress management. In U.S. cities like Loma Linda, California, where Blue Zone principles have been adopted, residents show lower rates of obesity and chronic diseases. This proves that cultural and community-driven approaches can reshape health outcomes when combined with education and infrastructure support.
7. Will Medicare cover preventive lifestyle medicine in the future?
There is growing momentum for Medicare to expand coverage for preventive lifestyle medicine. Currently, Medicare does cover screenings for conditions like diabetes, obesity counseling, and some wellness visits. However, more comprehensive coverage—such as fitness programs, nutritional coaching, and digital health tools—remains limited. Advocates argue that expanding preventive care could significantly reduce long-term costs and improve outcomes for aging Americans. If policy shifts align with public health goals, Medicare could play a leading role in combating the lifestyle disease epidemic.
8. Can workplace wellness programs significantly reduce healthcare costs?
Yes, workplace wellness programs can deliver substantial savings while improving employee health and morale. Studies show that for every dollar invested in wellness initiatives, employers can save up to three dollars in reduced healthcare expenses and productivity gains. Programs that combine fitness challenges, healthy food options, and mental health support are especially effective. For instance, Johnson & Johnson reported saving over $250 million in healthcare costs after a decade of wellness initiatives. These programs also enhance employee retention and job satisfaction.
9. What’s the link between mental health and lifestyle diseases?
Mental health is deeply connected to lifestyle diseases. Stress, anxiety, and depression often lead to unhealthy coping behaviors such as overeating, poor sleep, smoking, or alcohol use. Over time, these behaviors increase the risk of obesity, diabetes, and heart disease. Additionally, chronic illness can worsen mental health, creating a vicious cycle. Addressing both mental and physical health together—through therapy, mindfulness, and healthier routines—is crucial for breaking this cycle and reducing lifestyle disease risks.
10. How do U.S. lifestyle disease trends compare with Europe or Asia?
The U.S. has some of the highest obesity and diabetes rates in the developed world. While Europe and parts of Asia are also experiencing rising rates, their levels remain lower due to differences in diet, lifestyle, and healthcare systems. For example, Mediterranean countries prioritize fresh vegetables, olive oil, and daily activity, leading to lower heart disease rates. Asian nations, while urbanizing, still consume fewer processed foods than Americans. The U.S. can learn valuable lessons from these global models to shift its trajectory.
Conclusion: The Future Health of America Is a Choice
The lifestyle disease epidemic is not destiny—it is a choice. America has the knowledge, technology, and resources to reverse the trend. The next decade will be critical in deciding whether the U.S. embraces a prevention-first culture or continues down a costly and unhealthy path.
The good news? Every small step—whether by individuals, communities, or policymakers—brings the country closer to a healthier, more sustainable future.
Read this also : https://myhealthhacks.us/can-hypertension-be-reversed-naturally/