Gut health has become one of the most viral wellness topics, with claims linking it to immunity, mood, skin, and weight. But is “gut healing” just another buzzword? This in-depth critique explores science vs. hype, examines diet trends, busts myths, and provides practical, research-backed advice. Learn how your gut really affects your health, which fads to avoid, and what actually works.
Why Everyone’s Talking About Gut Healing
Scroll through TikTok or Instagram in 2025, and you’ll see influencers touting “gut reset challenges,” “detox teas,” or miracle diets promising to heal your digestive system in a week. Celebrities endorse probiotic gummies. Health coaches sell e-books with “gut-healing meal plans.”
But here’s the million-dollar question: Is “gut healing” a legitimate medical necessity or just another trendy buzzword repackaged for virality?
The truth lies somewhere in between. While science confirms the gut’s role in immunity, metabolism, and mental health, many viral diets oversimplify or outright misrepresent this connection. This article unpacks the real science of gut health, critiques common viral trends, and provides practical, trustworthy strategies backed by experts.
What Does “Gut Healing” Even Mean?
Unlike medical diagnoses such as Irritable Bowel Syndrome (IBS) or Celiac Disease, “gut healing” isn’t a medically recognized condition. It’s a pop-culture term that refers to improving digestion, reducing bloating, and rebalancing the gut microbiome.
In reality, your gut is not “broken” unless you have a diagnosed condition. Instead, it may be imbalanced due to poor diet, stress, lack of sleep, or antibiotic overuse.
Key takeaway: Gut healing is less about “fixing damage” and more about supporting balance within the microbiome.
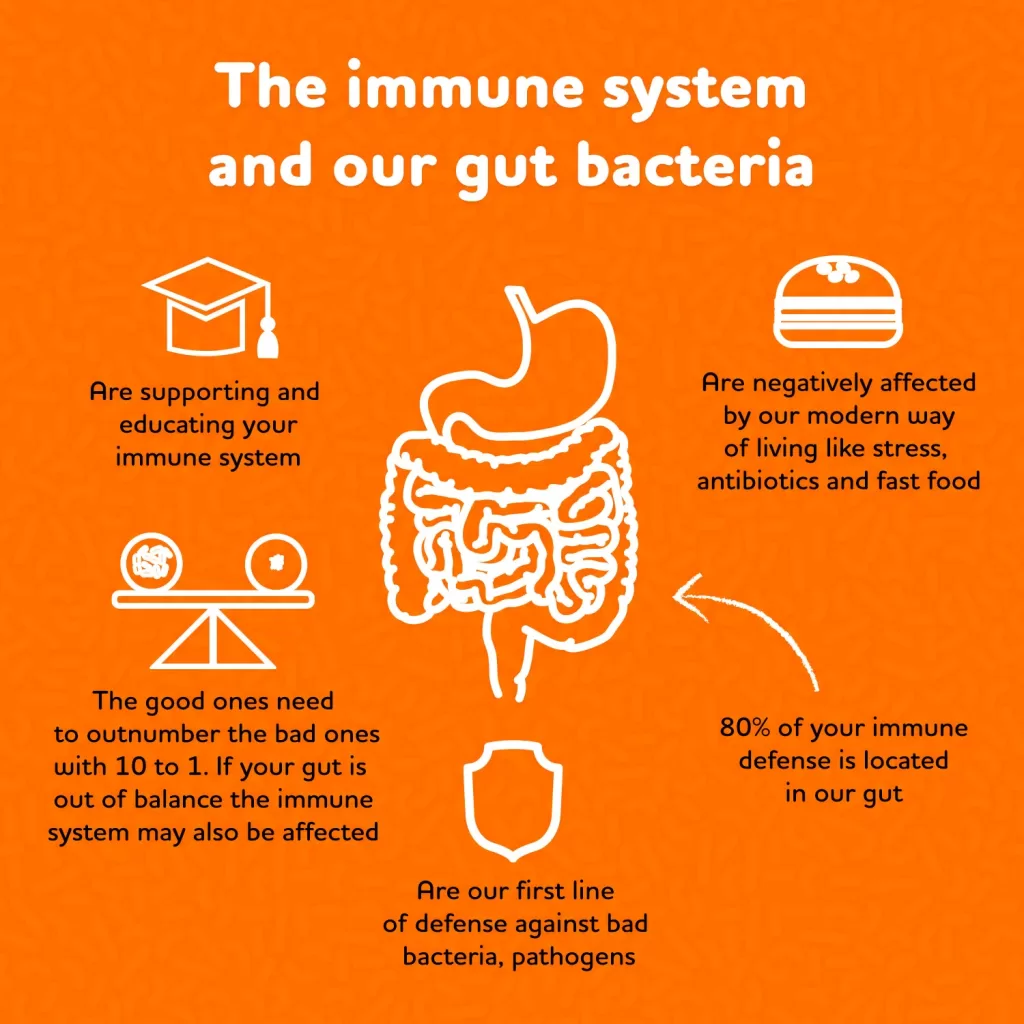
Is It True That 70% of Your Immune System Is in Your Gut?
Yes—approximately 70% of immune cells reside in the gastrointestinal tract, particularly in gut-associated lymphoid tissue (GALT). This means that what you eat, how you digest, and even your gut bacteria directly affect immune responses.
For example:
- A healthy gut microbiome helps regulate inflammation and prevents autoimmune reactions.
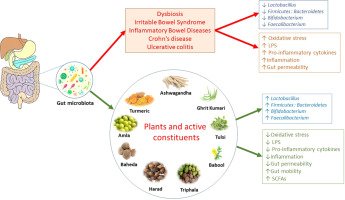
- Dysbiosis (imbalance of gut bacteria) is linked to allergies, asthma, and autoimmune conditions like Crohn’s disease.
- Fiber-rich diets strengthen the gut barrier, making you less vulnerable to infections.
Practical tip: Rather than buying “immune-boosting” supplements, focus on whole foods that support microbial diversity—vegetables, fruits, legumes, and fermented foods.

The 3 F’s of Gut Health
Nutritionists often recommend remembering the “3 F’s” to keep gut health simple and practical:
- Fiber – feeds beneficial gut bacteria and supports regularity.
- Example: Oats, beans, apples.
- Fermented Foods – add probiotics that strengthen the gut microbiome.
- Example: Yogurt, kimchi, sauerkraut.
- Fluids – hydration aids digestion and prevents constipation.
- Example: Water, herbal teas, diluted fruit-infused water.
These basics are far more sustainable than expensive cleanses or supplements.
Viral Diet Trends That Claim to Heal the Gut (And the Truth Behind Them)
1. Juice Cleanses and Detox Teas
- The Claim: Flush out toxins, reset your gut.
- The Reality: The liver and kidneys detox naturally. Juice cleanses often strip fiber, ironically starving good gut bacteria.
2. Low-FODMAP Diet
- The Claim: Reduces bloating and IBS symptoms.
- The Reality: Helpful for diagnosed IBS, but overly restrictive for the average person. Best used short-term with a dietitian.
3. Gluten-Free for All
- The Claim: Gluten inflames the gut, so cutting it heals digestion.
- The Reality: True only for celiac or gluten sensitivity. Unnecessary restriction can reduce whole-grain fiber intake.
4. Collagen Powders and Bone Broth
- The Claim: Seal a “leaky gut.”
- The Reality: Collagen supports skin and joints, but evidence on gut lining repair is weak. Bone broth may be nutritious but not a magic fix.
5. Probiotic Pills
- The Claim: Instantly restore gut balance.
- The Reality: Some strains help with diarrhea or IBS, but benefits vary. Food-based probiotics are more reliable long-term.
Real-Life Stories: When Gut Health Is Misunderstood
- Case 1: The Trend Follower
Sarah, 28, followed a “7-day gut reset” she found online. After cutting carbs and eating only bone broth and teas, she felt dizzy, irritable, and gained weight back in weeks. - Case 2: The Balanced Approach
Michael, 45, had chronic bloating. Instead of fad diets, he added oats, yogurt, and more vegetables while cutting back on processed foods. Within 3 months, his digestion and energy improved.
These stories highlight why slow, evidence-based changes outperform extreme diet hacks.
How Do Stress and Sleep Affect Gut Health?
Your gut and brain are connected via the gut-brain axis. Stress releases cortisol, which alters gut motility and microbiota composition. Poor sleep has a similar effect.
- High stress → bloating, diarrhea, or constipation
- Low sleep → reduced beneficial bacteria
Actionable tip: Meditation, yoga, and consistent sleep schedules may “heal” your gut as effectively as dietary changes.
FAQs About Gut Healing
1. Is gut healing a myth or reality?
Gut healing is not a medical diagnosis, but it is not entirely a myth either. The term “gut healing” has been popularized on social media and wellness platforms, often used as a buzzword to market supplements, cleanses, and restrictive diets. In reality, what people are referring to is the concept of improving gut microbiome balance and restoring gut lining integrity.
The reality is that the gut is dynamic—it repairs itself naturally when supported with adequate nutrition, hydration, and rest. For example, your intestinal lining regenerates every 3–5 days. That means your body already has powerful repair mechanisms built in. What does help is removing irritants (ultra-processed foods, excessive alcohol, chronic stress) and adding nourishing inputs (fiber, probiotics, whole foods).
So while “gut healing” in the influencer sense may be exaggerated, the underlying principle—that you can strengthen your gut through diet and lifestyle—is absolutely real.
2. How long does it take to heal your gut?
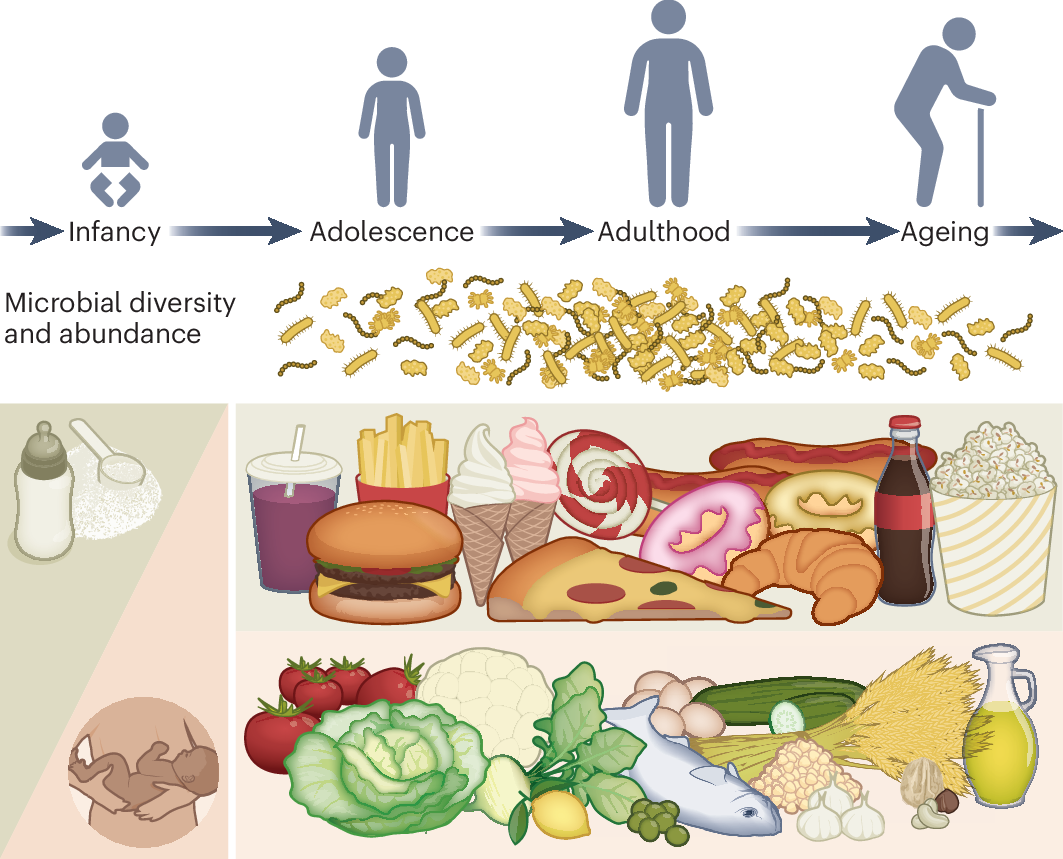
There is no universal timeline, because gut health depends on genetics, diet, stress, and medical conditions. However, research shows that meaningful changes in the microbiome can occur within days of dietary shifts, while deeper balance may take 3–6 months of consistency.
- Short-term changes (within 48 hours): If you switch from fast food to a fiber-rich diet, your microbiota composition can start to shift quickly.
- Medium-term changes (4–12 weeks): Regular consumption of prebiotics (fiber), fermented foods, and better sleep patterns often improve digestion and reduce bloating.
- Long-term changes (6 months to 1 year): This is when individuals report sustained improvement in immunity, skin clarity, and energy levels.
Takeaway: Gut healing isn’t a “7-day reset.” It’s a lifestyle pattern that requires patience and consistency.
3. Do antibiotics ruin your gut?
Antibiotics can significantly disrupt gut bacteria, but the effects are not necessarily permanent. A single course may wipe out up to 30% of microbial diversity, reducing both beneficial and harmful strains. This disruption can lead to short-term issues like diarrhea, bloating, or yeast overgrowth.
Recovery depends on several factors:
- Diet after antibiotics: Eating plenty of fiber (legumes, oats, fruits, vegetables) helps re-seed beneficial bacteria.
- Probiotics: Clinical studies suggest that targeted strains like Lactobacillus rhamnosus GG can reduce antibiotic-associated diarrhea.
- Time: Many people regain balance within 3–6 months, but frequent antibiotic use can have cumulative effects.
So no, antibiotics don’t permanently “ruin” your gut—but they do highlight the importance of supporting your microbiome during and after treatment.
4. Can poor gut health cause skin issues?
Yes. The gut-skin axis is a well-documented phenomenon. When your gut bacteria are imbalanced (dysbiosis), it can trigger systemic inflammation that often appears on the skin. For instance:
- Acne: Linked to excess gut permeability and inflammatory diets high in sugar.
- Eczema and Psoriasis: Associated with reduced microbial diversity and overactive immune responses.
- Rosacea: Research suggests an overgrowth of certain gut bacteria contributes to flare-ups.
Real-life example: Many people who reduce processed sugars and increase prebiotic foods (onions, bananas, garlic) notice their acne improves. Dermatologists are increasingly collaborating with gastroenterologists to treat skin flare-ups holistically.
5. Does fasting improve gut health?
Intermittent fasting has gained attention not just for weight management, but also for gut health. Studies suggest that fasting periods may allow the gut lining to repair, reduce inflammation, and promote microbial diversity. Some people report reduced bloating and improved bowel regularity with time-restricted eating.
However, extreme fasting or long-term starvation can have the opposite effect, leading to loss of gut lining integrity and bacterial imbalance. For example, prolonged calorie restriction reduces short-chain fatty acids (SCFAs) that protect the gut barrier.
So while moderate intermittent fasting (12–16 hours) may support gut balance, extreme fasting diets promoted online are not sustainable or safe for everyone.
6. Can kids have poor gut health?
Absolutely. Children raised on ultra-processed foods high in sugar and additives may experience reduced microbial diversity early in life. This can contribute to frequent infections, allergies, and digestive complaints. Overuse of antibiotics in childhood is another factor that can weaken gut resilience.
To support a child’s gut:
- Offer a variety of colorful fruits and vegetables.
- Introduce fermented foods like yogurt early (if tolerated).
- Limit sugary snacks and sodas.
- Encourage outdoor play, as exposure to natural microbes strengthens immunity.
Parents should consult pediatricians before adding supplements. The best gift for a child’s gut is a balanced diet and lifestyle, not fads.
7. What are signs of poor gut health?
Some symptoms are obvious, while others are more subtle. The most common include:
- Chronic bloating, gas, constipation, or diarrhea
- Unexplained fatigue
- Frequent infections (low immunity)
- Food intolerances or sensitivities
- Mood changes like anxiety or irritability
- Skin flare-ups
It’s important to note that these symptoms can overlap with other conditions, so a professional diagnosis is crucial. For example, constant bloating might indicate IBS, SIBO (small intestinal bacterial overgrowth), or lactose intolerance—not just a “gut imbalance.”
8. Is gut healing linked to weight loss?
Indirectly, yes. A diverse gut microbiome helps regulate metabolism, appetite, and fat storage. Some bacteria are associated with leanness (Akkermansia muciniphila), while others are linked to obesity when overgrown.
However, no single probiotic or cleanse guarantees fat loss. Instead, improving gut balance may:
- Reduce sugar cravings
- Improve insulin sensitivity
- Normalize bowel movements, reducing bloating
Realistic expectation: Gut support can help with weight management, but it is not a magic fat-loss tool. Sustainable lifestyle habits matter far more.
9. Should you take probiotics daily?
It depends on your health status and diet. For healthy individuals with a balanced diet, probiotics from fermented foods (yogurt, kefir, sauerkraut) may be sufficient. For those with IBS, antibiotic recovery, or chronic diarrhea, targeted supplements may be beneficial.
But probiotics are not one-size-fits-all. The strain, dose, and duration matter. For example:
- Saccharomyces boulardii is effective against traveler’s diarrhea.
- Lactobacillus plantarum may reduce bloating.
The best approach is to experiment with food-based probiotics first, and consult a healthcare professional before long-term supplementation.
10. Are gut health supplements worth it?
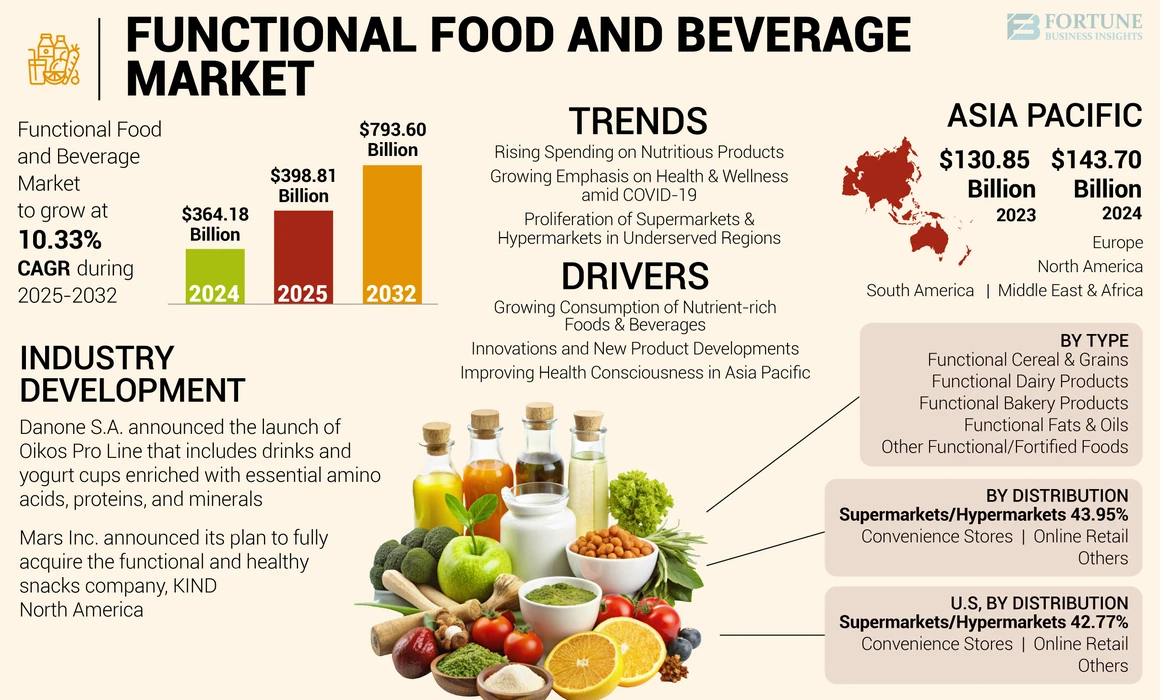
The gut health supplement industry is booming, with powders, capsules, and “gut-healing kits” often priced at premium levels. While some products have supportive research, many are overhyped.
Worth considering:
- High-quality probiotics with clinically studied strains
- Prebiotic fibers (like inulin or psyllium husk)
- Omega-3 supplements (support anti-inflammatory pathways)
Often unnecessary:
- “Leaky gut” powders with collagen and glutamine (research is inconclusive)
- Expensive enzyme blends (unless prescribed for pancreatic issues)
In most cases, a whole-foods diet, stress management, and good sleep outperform supplements. Supplements should be supportive, not central, to your gut health strategy.
Expert-Backed Advice for Supporting Gut Health
- Eat a variety of plant-based foods weekly (aim for 30+ different plants).
- Limit ultra-processed foods high in refined sugars and additives.
- Incorporate fermented foods like kefir or kombucha.
- Manage stress with breathing exercises or journaling.
- Stay hydrated and prioritize consistent sleep.
Final Thoughts: Buzzword or Breakthrough?
“Gut healing” as a phrase may be overhyped, but the science of gut health is very real. Americans don’t need detox teas or trendy cleanses—they need consistency in food, sleep, and stress management.
The real takeaway? You can’t hack your gut overnight. But you can support it for life with balance, patience, and evidence-based choices.