Measles cases are surging across the U.S. and globally in 2025, raising fears of a public health crisis. Discover why this preventable disease is back, what it means for your family, and how to protect yourself with trusted resources and expert insights.
Measles, once nearly eradicated, is staging a dangerous comeback in the U.S. and globally due to falling vaccination rates, misinformation, and global travel. This resurgence is straining public health systems and igniting fears of a new epidemic. In this article, we explore why measles is back, the real risks to children and communities, prevention strategies, and what policymakers and families must do now.
Why Measles Is Back in the Spotlight
Not long ago, measles was thought to be a disease of the past. By 2000, the United States declared it eliminated thanks to widespread vaccination. Yet in 2025, headlines warn of outbreaks in multiple states, hospital wards filling up with preventable cases, and the Centers for Disease Control and Prevention (CDC) sounding alarms.
This resurgence is not just a matter of numbers—it signals a public health crisis fueled by vaccine hesitancy, misinformation, and gaps in global immunization coverage. The question is no longer “Is measles back?” but “Are we ready to stop it before it becomes a national epidemic?”

Measles Outbreak Statistics in 2025
- Global Rise: According to the World Health Organization (WHO), measles cases rose by 79% worldwide in 2024 compared to the year prior.
- U.S. Outbreaks: As of mid-2025, more than 1,200 confirmed cases have been reported across 20 states, compared to fewer than 400 cases annually in the late 2010s.
- Severe Outcomes: Measles causes complications such as pneumonia, encephalitis, and even death—especially in children under five.
Resource: WHO Measles Fact Sheet
Why Is Measles Making a Comeback?
1. Declining Vaccination Rates
One of the biggest drivers is reduced uptake of the MMR vaccine (Measles, Mumps, Rubella). Vaccine hesitancy has surged due to:
- Spread of misinformation on social media.
- Distrust in government health institutions.
- Disruptions caused by the COVID-19 pandemic.
2. Global Travel and Importation of Cases
Even if vaccination coverage is high in the U.S., travelers can bring measles from countries experiencing outbreaks. Just one imported case can trigger community spread where local immunity is weak.
3. Waning Public Awareness
Because measles was nearly eradicated for decades, many young parents have never seen it firsthand. This has created a false sense of security.
4. Underfunded Public Health Infrastructure
Some states have under-resourced vaccination campaigns, leaving vulnerable communities unprotected.
Real-Life Example: The Disneyland Outbreak
In 2015, Disneyland in California became the epicenter of a measles outbreak, infecting 147 people across seven states. Fast forward to 2025, experts fear that similar events could happen at concerts, sports arenas, or schools if vaccination gaps persist.
The Public Health Crisis Explained
The term “crisis” is not used lightly. Here’s why measles resurgence is more than a medical issue—it’s a social and economic threat:
- Hospital Strain: Measles patients require isolation and intensive care, stretching hospital resources.
- Economic Cost: Outbreaks cost millions in emergency response, contact tracing, and productivity loss.
- Community Spread: Unvaccinated groups (children, travelers, marginalized populations) act as hotspots.
- Erosion of Trust: Ongoing outbreaks damage confidence in public health systems.
How Dangerous Is Measles for Children and Adults?
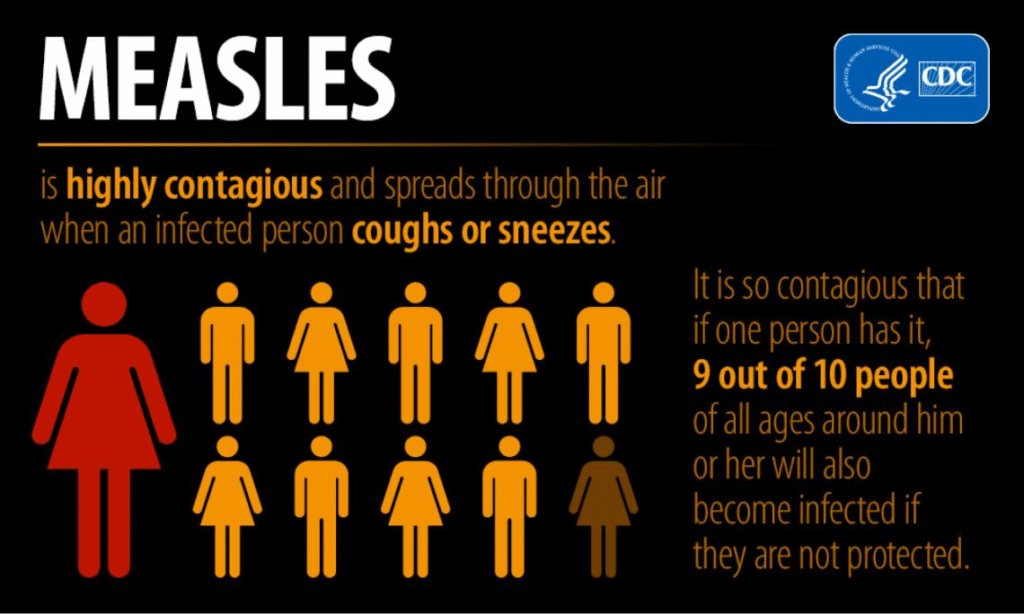
Measles is not a “mild childhood illness.” It is highly contagious—one person can infect up to 18 others.
Complications include:
- Pneumonia (most common cause of measles-related deaths).
- Brain swelling (encephalitis).
- Blindness or hearing loss.
- Miscarriage or premature birth in pregnant women.
In the U.S., about 1–2 in every 1,000 children who contract measles die from complications.
What Can Families Do Right Now?
- Check Vaccination Records: Ensure all family members have received both doses of the MMR vaccine.
- Stay Informed: Follow updates from the CDC and local health departments.
- Travel Wisely: If traveling internationally, get vaccinated at least 2 weeks before departure.
- Educate Others: Share evidence-based resources, not myths.
Top Questions Americans Are Asking About Measles
1. Is measles making a comeback in the U.S.?
Yes. Outbreaks are being reported in multiple states, with CDC confirming a steep rise in cases since 2023.
2. Why are vaccination rates dropping?
Vaccine misinformation and pandemic-era disruptions caused many children to miss scheduled immunizations.
3. How do I know if I or my child is protected?
Most people need two doses of the MMR vaccine. Your doctor can run a blood test for immunity if records are unclear.
4. Can adults get measles?
Yes. Adults born after 1957 who were never vaccinated remain at risk. Recent outbreaks show adults are also affected.
5. Is measles deadly?
Yes. It is one of the world’s leading causes of death among children, despite being preventable.
6. What are early symptoms of measles?
High fever, cough, runny nose, red eyes, and tiny white spots in the mouth (Koplik spots) before rash appears.
7. Can vaccinated people still get measles?
Breakthrough infections are rare, but possible. Vaccinated individuals usually experience much milder symptoms.
8. How is measles spread?
Through coughing, sneezing, or even breathing in a space where an infected person was—virus particles linger for 2 hours.
9. Is measles worse than COVID-19?
Measles is more contagious than COVID-19 but has an effective vaccine that prevents nearly all cases.
10. What should I do if exposed to measles?
Call your doctor immediately. Vaccination within 72 hours or immune globulin treatment may prevent illness.
Key Takeaways
- Measles is resurging in the U.S. and globally in 2025.
- Falling vaccination rates and misinformation are primary causes.
- The disease is highly contagious and dangerous, especially for children.
- Prevention through vaccination is safe, effective, and widely available.
- Public health action is critical to avoid another full-blown epidemic.