Summary
Obesity in America has reached alarming levels, with nearly 42% of U.S. adults classified as obese according to the CDC. This silent epidemic drives rising healthcare costs, lowers workforce productivity, and shortens life expectancy. The causes range from sedentary lifestyles and processed diets to socioeconomic factors. This article explores why obesity is rising, its impact on health and the economy, and what strategies can help Americans combat this growing crisis.
Introduction: Why Is Obesity Called America’s Silent Epidemic?
Obesity doesn’t always grab headlines like pandemics or economic recessions, but its effects are just as damaging—and longer lasting. With nearly half of Americans classified as obese, this epidemic silently erodes quality of life, strains the healthcare system, and undermines workforce efficiency.
Unlike sudden outbreaks, obesity develops gradually, influenced by diet, environment, and cultural factors. That’s why health experts call it a “silent epidemic”—one that grows unnoticed until its devastating consequences manifest in heart disease, diabetes, and reduced life expectancy.
How Prevalent Is Obesity in the United States?
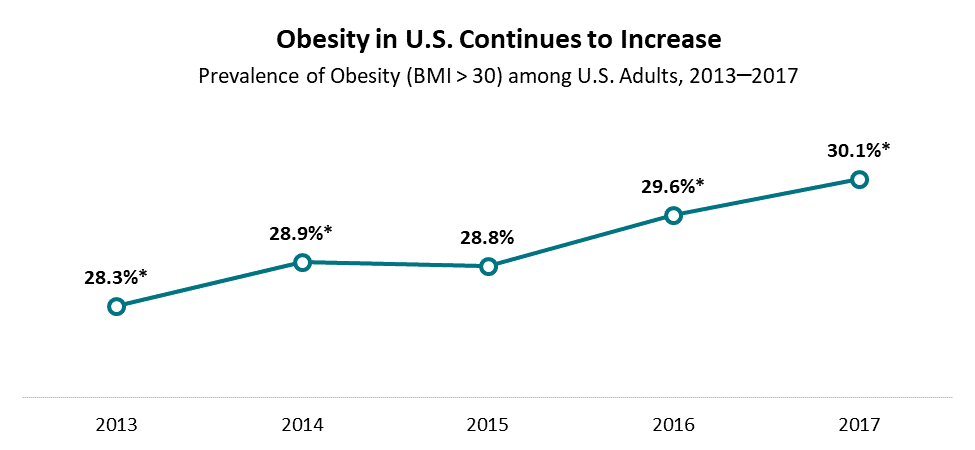
According to the Centers for Disease Control and Prevention (CDC), adult obesity prevalence in the U.S. climbed from 30.5% in 2000 to 42.4% in 2018, and the trajectory continues upward. Childhood obesity has also tripled since the 1970s, affecting nearly 1 in 5 children.
This isn’t just a health statistic; it’s an urgent wake-up call. If trends continue, some projections suggest half of U.S. adults could be obese by 2030.
What Factors Are Driving America’s Obesity Epidemic?
The causes of obesity in the U.S. are multifaceted. Key contributors include:
- Sedentary Lifestyle: With remote work and digital entertainment, physical activity has plummeted. The average American adult spends more than 7 hours per day sitting.
- Ultra-Processed Diets: Fast food, sugary drinks, and packaged snacks dominate the American diet. Nearly 60% of calories consumed in the U.S. come from ultra-processed foods.
- Socioeconomic Inequality: Low-income communities often lack access to fresh produce, making cheap, high-calorie foods the default.
- Cultural Norms: Portion sizes in the U.S. are significantly larger than in most countries, normalizing overeating.
- Mental Health: Stress, anxiety, and depression contribute to emotional eating and poor nutrition choices.
How Does Obesity Affect the Health of Americans?
Obesity is not just about body image; it’s a chronic disease with life-threatening complications.
- Cardiovascular Disease: Obesity increases risks of hypertension, stroke, and heart attack.
- Type 2 Diabetes: Nearly 90% of people with Type 2 diabetes are overweight or obese.
- Cancer: Certain cancers (colon, breast, endometrial) have strong links to obesity.
- Respiratory Issues: Obesity exacerbates conditions like sleep apnea and asthma.
- Mental Health: Obesity contributes to depression, stigma, and reduced self-esteem.
Real-life example: In a 2023 study published in JAMA, researchers found that obesity reduced average U.S. life expectancy by nearly 4 years, primarily due to chronic disease complications.
What Is the Economic Cost of Obesity in the U.S.?
The financial toll is staggering. According to the CDC, obesity costs the U.S. healthcare system nearly $173 billion annually.
- Direct Costs: Hospital care, medications, and treatments for obesity-related diseases.
- Indirect Costs: Lost productivity, absenteeism, and disability claims.
- Employer Burden: Obese employees generate nearly $1,400 more in annual medical costs compared to those of healthy weight.
The ripple effect extends beyond healthcare, affecting GDP growth, workforce readiness, and even national security—since obesity is now one of the leading reasons young Americans are deemed unfit for military service.
How Does Childhood Obesity Impact Future Generations?
Childhood obesity has become one of the most alarming trends in U.S. public health. Children with obesity are more likely to:
- Develop chronic diseases at younger ages.
- Struggle with mental health issues due to bullying and stigma.
- Become obese adults, perpetuating the cycle.
Example: A child diagnosed with obesity at age 10 has an 80% likelihood of remaining obese into adulthood unless interventions are made.
Are Fast Food and Processed Foods to Blame?
The American diet is one of the largest drivers of the obesity epidemic. Fast food chains and processed snacks dominate the market with affordable, calorie-dense meals.
- Portion Inflation: A soda in the 1950s was 6 ounces; today, a “medium” is often 20 ounces.
- High-Fructose Corn Syrup: Widely used in U.S. beverages, linked to weight gain and diabetes.
- Marketing to Children: Over $1.7 billion is spent annually advertising unhealthy foods to kids.
What Role Does Technology Play in Rising Obesity Rates?
While technology enables health-tracking apps and virtual workouts, it also fuels sedentary behavior.
- Streaming & Gaming: Binge-watching TV and gaming marathons replace physical play.
- Remote Work: Post-pandemic, millions of Americans work from home, often moving less.
- Food Delivery Apps: Easy access to fast food at the tap of a screen normalizes poor diet habits.
Can Public Policy Help Curb Obesity?
Yes, policy interventions can make a difference. Examples include:
- Soda Taxes: Cities like Philadelphia introduced soda taxes, resulting in reduced sugary drink purchases.
- School Nutrition Programs: The Healthy, Hunger-Free Kids Act improved school lunches by adding more fruits, vegetables, and whole grains.
- Zoning Laws: Some cities restrict fast food outlets near schools.
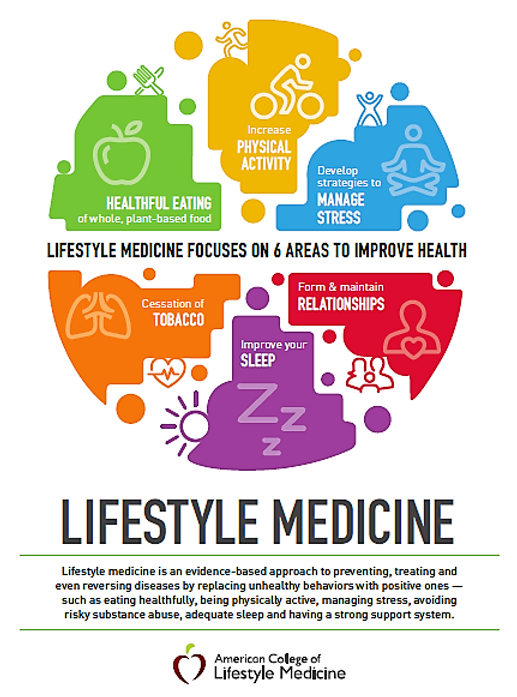
Practical Steps for Americans to Tackle Obesity
While the epidemic is complex, individuals can take actionable steps:
- Adopt the 80/20 diet rule (80% whole foods, 20% flexibility).
- Aim for at least 150 minutes of physical activity per week.
- Reduce screen time by setting digital wellness goals.
- Use wearable tech like Fitbit or Apple Watch to stay accountable.
- Seek community-based support programs.
FAQs: Rising Obesity Rates in America
1. Why are obesity rates in the U.S. higher than in other countries?
Obesity rates are higher in the U.S. due to a combination of factors: portion sizes, reliance on ultra-processed foods, sedentary lifestyles, and urban planning that often discourages walking or biking. Additionally, aggressive food marketing and socioeconomic disparities limit access to healthier choices for many Americans.
2. How does obesity affect life expectancy in the United States?
Research shows obesity shortens life expectancy by several years due to complications like diabetes, heart disease, and cancer. For instance, a person with severe obesity may live 5–10 years less than someone of a healthy weight. The overall impact is a decline in U.S. life expectancy compared to other developed nations.
3. Is childhood obesity reversible?
Yes, childhood obesity is reversible with early intervention. Lifestyle changes such as balanced diets, increased physical activity, and supportive family habits can significantly reduce risks. Pediatric healthcare providers often stress early treatment since the likelihood of reversing obesity decreases as children grow older.
4. Do genetics play a role in obesity?
Genetics influence metabolism and fat storage, but lifestyle and environment remain the primary drivers of obesity. For example, even if a child has a genetic predisposition, a healthy diet and active lifestyle can greatly reduce their risk of becoming obese.
5. How much does obesity cost U.S. taxpayers?
Obesity costs the U.S. healthcare system $173 billion annually, including both direct and indirect costs. Taxpayers bear much of this burden through Medicare and Medicaid expenses, highlighting the need for public health solutions.
6. Can apps and technology help combat obesity?
Yes, technology can help by promoting accountability. Fitness apps, meal trackers, and virtual workout classes are valuable tools. However, these are only effective if paired with consistent lifestyle changes, not as stand-alone solutions.
7. Are food deserts contributing to obesity in America?
Absolutely. Food deserts—areas with limited access to affordable, nutritious food—force communities to rely on fast food and convenience stores. Studies show residents of food deserts are more likely to develop obesity and related chronic diseases.
8. What role do schools play in addressing obesity?
Schools play a vital role by offering healthy meals, physical education, and health education programs. Policies like banning soda machines and integrating farm-to-table lunch programs have shown measurable benefits in reducing obesity among students.
9. Why is obesity considered a national security issue?
Obesity is now one of the top reasons young Americans are disqualified from military service. Nearly 1 in 3 young adults is too overweight to enlist, raising concerns about the future readiness of U.S. armed forces.
10. What is the most effective long-term strategy to reduce obesity?
The most effective strategies involve multi-level approaches: personal lifestyle changes, family support, community programs, and public policy. A mix of healthier food access, regular exercise, education, and government incentives is necessary to curb obesity long-term.
Conclusion: Can America Reverse the Obesity Epidemic?
Obesity is not just a personal health issue—it’s a collective crisis impacting the nation’s health, economy, and future. While reversing the epidemic won’t happen overnight, coordinated efforts between individuals, communities, policymakers, and the private sector can create real change. Addressing obesity requires reshaping environments, improving food access, and building healthier cultural norms. With awareness and action, America can move from silent suffering to visible progress.
Read this also : https://myhealthhacks.us/is-fast-food-the-biggest-risk-to-modern-health/