In the landscape of American healthcare, seeking help for mental wellness often feels like trying to read a map in a language you don’t understand, while carrying a heavy, invisible weight. The decision to prioritize your psychological well-being is a courageous first step, but it is frequently met with a daunting reality: a labyrinthine system fraught with financial barriers, bureaucratic hurdles, and profound stigma. The “cost of caring” is not merely a financial figure on a bill; it is a multi-faceted burden comprising time, energy, emotional labor, and societal pressure.
This article is a guide for that journey. It is written from a place of deep understanding—not just of the system’s mechanics, but of the human experience within it. We will dissect the complexities of the U.S. healthcare system as it pertains to mental health, offering a clear, authoritative, and trustworthy roadmap. Our goal is to empower you with the knowledge and strategies to secure the care you deserve, transforming a path of frustration into one of informed, proactive navigation.
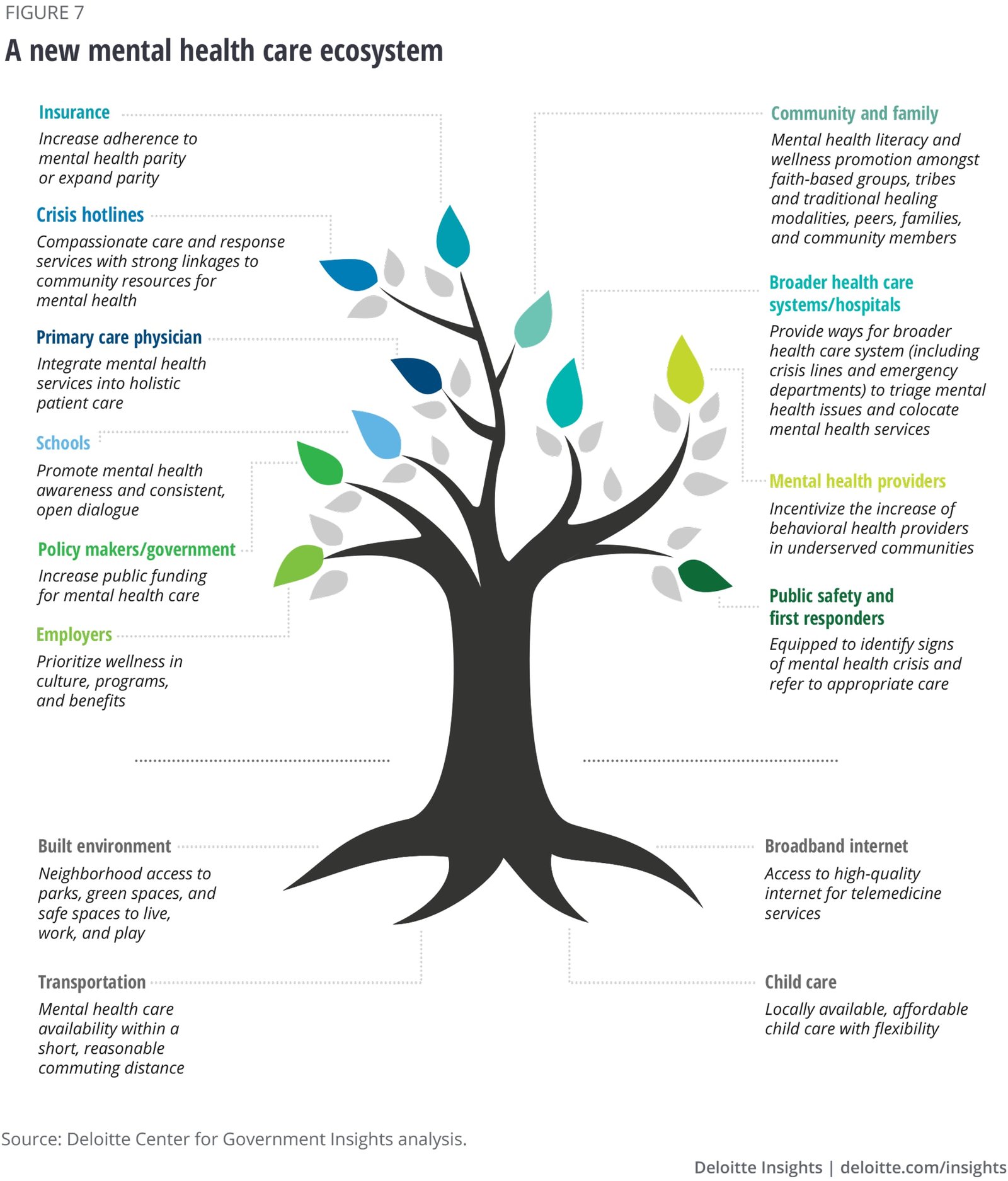
Part 1: Understanding the Landscape – The System and Its Stakeholders
Before you can navigate the system, you must understand its core components and the key players involved. This foundational knowledge is critical to making informed decisions.
1.1 The Pillars of Mental Healthcare Delivery
Mental health care in the U.S. is not a monolithic entity. It is delivered through several distinct, and sometimes overlapping, channels:
- Primary Care Providers (PCPs): For many Americans, the first point of contact for a mental health concern is their family doctor or internist. PCPs are skilled at conducting initial screenings for conditions like depression and anxiety and can prescribe common medications (e.g., SSRIs). However, their expertise has limits, and they often serve as a crucial referral source to specialized care.
- Outpatient Therapists and Counselors: This is the most common form of talk therapy. Providers can include:
- Psychologists (PhD or PsyD): Hold doctoral degrees and specialize in psychological testing, diagnosis, and psychotherapy. They typically cannot prescribe medication.
- Licensed Clinical Social Workers (LCSW), Licensed Professional Counselors (LPC), and Marriage and Family Therapists (LMFT): Master’s-level clinicians trained in providing psychotherapy for individuals, couples, and families.
- Psychiatrists (MD or DO): Medical doctors who specialize in the diagnosis and treatment of mental health disorders. Their unique qualification is the ability to prescribe medication. Many also provide psychotherapy, though the trend is shifting towards medication management alongside a therapist.
- Inpatient and Residential Treatment: This is the highest level of care, designed for individuals experiencing acute crises that pose a danger to themselves or others, or who require 24/7 stabilization. This includes psychiatric hospitals and residential treatment centers for conditions like severe eating disorders or substance use.
- Community Mental Health Centers (CMHCs): Federally funded facilities that provide care on a sliding-scale basis, making services more accessible to those with limited financial means or public insurance. They offer a range of services, from therapy to case management.
- Digital and Telehealth Platforms: The rapid growth of companies like BetterHelp, Talkspace, and Cerebral has created a new avenue for access. These platforms connect users with licensed therapists via video, phone, or text. While they increase convenience and can reduce stigma, they also come with unique considerations regarding insurance coverage, privacy, and the depth of the therapeutic relationship.
1.2 The Key Players: Who Controls Your Access?
- Insurance Companies (Payers): Whether private (e.g., Blue Cross Blue Shield, UnitedHealthcare) or public (Medicare, Medicaid), insurers are gatekeepers. They determine which providers are “in-network,” what services are covered, the rate of reimbursement, and require pre-authorizations for certain treatments. Understanding your insurer’s role is non-negotiable.
- Employers: For the majority of Americans with private insurance, their employer selects the health plans on offer. Your employer’s chosen plan directly dictates your mental health benefits, network size, and out-of-pocket costs.
- Providers (Clinicians): The individuals who deliver care. Their credentials, specialties, therapeutic approaches, and whether they accept your insurance are paramount to your choice.
- You (The Consumer/Patient): You are the most important player in this system. Being a proactive, informed advocate for your own care is the single most powerful factor in achieving a positive outcome.
Part 2: Decoding the Financial Maze – The True “Cost” of Caring
The financial burden of mental healthcare is often the most significant barrier. Understanding the terminology and structure of costs is the first step toward managing them.
2.1 The Language of Cost: A Glossary
- Premium: The monthly fee you pay to your insurance company to maintain your coverage, regardless of whether you use services.
- Deductible: The amount you must pay out-of-pocket for covered services before your insurance begins to pay. A high-deductible plan means lower premiums but higher initial costs for care.
- Copayment (Copay): A fixed, flat fee you pay for a specific service at the time of care (e.g., $30 for a therapy session).
- Coinsurance: A percentage of the cost of a service that you pay after you’ve met your deductible (e.g., you pay 20% of a $150 session, which is $30, while insurance pays the remaining 80%).
- Out-of-Pocket Maximum: The absolute limit you will have to pay for covered services in a plan year. After you spend this amount through deductibles, copayments, and coinsurance, your insurance pays 100% of covered benefits.
2.2 The Affordability Crisis: Why Does Therapy Cost So Much?
A standard therapy session can range from $100 to $250 or more without insurance. Several factors drive this cost:
- Provider Education and Overhead: Clinicians have advanced, expensive degrees and must cover costs like office rent, malpractice insurance, electronic health record systems, and billing staff.
- Insurance Reimbursement Rates: Insurance companies negotiate lower rates with in-network providers. To sustain their practice, providers must set their self-pay (“cash”) rate higher.
- Time-Intensive Nature: Unlike a quick physical exam, therapy requires a full 45-60 minutes of a highly trained professional’s undivided attention.
2.3 Strategies for Managing Financial Burden
- Leverage Your Insurance: Before booking an appointment, call the number on the back of your insurance card. Ask specific questions:
- “Do I have mental health benefits?”
- “What is my copay/coinsurance for outpatient therapy with an in-network provider?”
- “What is my deductible, and has any of it been met?”
- “Do I need a referral from my PCP?”
- “Is pre-authorization required for therapy?”
- Explore Sliding Scale Options: Many private practice therapists reserve a certain number of slots for clients who pay on a sliding scale based on income. Don’t be afraid to ask a potential therapist if this is an option.
- Utilize Training Clinics: Universities with clinical psychology, counseling, or social work programs often have training clinics where graduate students provide therapy under close supervision by licensed faculty. These services are typically offered at very low cost.
- Investigate Employee Assistance Programs (EAPs): Your employer’s EAP is a tremendous, and often underutilized, benefit. It typically offers a set number of free, confidential counseling sessions (often 3-8) per issue, per year. This can be a great way to get immediate support and a referral for ongoing care.
- Consider Group Therapy: Group therapy, led by a trained professional, is significantly less expensive than individual therapy and provides the unique benefit of peer support and universality.
- Look into Open Path Psychotherapy Collective: This is a non-profit network of mental health professionals who offer sessions at a reduced rate ($40-$70) for individuals in financial need.
Part 3: The Practical Navigator – A Step-by-Step Guide to Securing Care
Knowledge is power, but action is results. This step-by-step guide translates understanding into practice.
Step 1: Self-Assessment and Acknowledgment
Before you dive into directories and phone calls, take a moment for introspection. What are you struggling with? (e.g., persistent sadness, panic attacks, relationship issues). What are your goals for therapy? (e.g., develop coping skills, process trauma, improve communication). Having a general sense of this will help you communicate your needs effectively.
Step 2: Verify Your Insurance and Benefits
This is the non-negotiable homework. Conduct the insurance interrogation outlined in Part 2.3. Get a clear picture of your financial responsibility.
Step 3: Find Potential Providers
- Insurance Provider Directory: Use your insurer’s online search tool to find in-network mental health providers. Warning: These directories are notoriously outdated. Always call the provider’s office to confirm they are still in-network with your plan.
- Therapist Directories: Websites like Psychology Today, TherapyDen, and GoodTherapy allow you to filter by location, insurance, specialty, gender, and therapeutic approach (e.g., CBT, EMDR, psychodynamic). These profiles often include photos and personal statements, helping you gauge a potential fit.
- Ask for Referrals: Your PCP, a trusted friend, or a clergy member can be excellent sources of recommendations.
Step 4: The Consultation Call – Your Screening Tool
Treat the initial phone call or email as a two-way interview. Prepare a short list of questions:
- “Are you currently accepting new clients and do you accept my insurance, [Insurance Name]?”
- “What is your experience and approach to treating [your concern, e.g., anxiety]?”
- “What does a typical session with you look like?”
- “What are your fees and availability?”
Pay attention to how you feel during the interaction. Do you feel heard and respected? The therapeutic relationship is built on trust and rapport, and this starts with the first contact.
Step 5: The First Appointment and Beyond
The first session is an intake, where the therapist will ask many questions to understand your history and current situation. It’s also your chance to ask more questions. It’s okay if the first therapist isn’t the right fit. A good therapist will not be offended if you decide to seek a better match and may even help you with a referral.
Step 6: Understanding Your Rights: The Mental Health Parity and Addiction Equity Act (MHPAEA)
This is a critical piece of federal law. In short, MHPAEA requires most insurance plans to offer mental health and substance use disorder benefits that are no more restrictive than their medical/surgical benefits. This means:
- They cannot charge higher copays or coinsurance for therapy than for a visit to a medical specialist.
- They cannot impose stricter limits on the number of visits.
- They cannot require more arduous prior authorization processes.
If you suspect your insurer is violating parity laws, you can file an appeal with them and a complaint with your state’s Department of Insurance.
Read more: The Soda, Sugar, and NAFLD Trio: America’s Growing (and Silent) Liver Disease Problem
Part 4: Special Considerations and Emerging Trends
The landscape of mental healthcare is not one-size-fits-all. Specific populations and new models require tailored understanding.
4.1 Navigating for a Loved One
When you are supporting a child, a partner, or an aging parent, the navigation challenges multiply.
- Minors: Consent for treatment must be provided by a parent or guardian. Family therapy is often involved. When searching for a provider, look for those who specialize in child and adolescent psychology.
- Adult Children/Elderly Parents: This often involves complex issues of capacity, consent, and Medicare. Understanding Medicare’s mental health coverage (Part B covers outpatient services with a 20% coinsurance after the deductible) is essential. Be prepared to advocate fiercely within medical and long-term care settings.
4.2 The Digital Frontier: Telehealth Pros and Cons
Telehealth has been a game-changer for accessibility, especially for those in rural areas or with mobility issues.
- Pros: Convenience, reduced travel time and cost, access to a wider pool of providers, comfort of being in your own space.
- Cons: Not ideal for crises; potential for technology glitches; privacy concerns; some therapeutic techniques are less effective remotely; state licensing laws mean your therapist must be licensed in the state where you are physically located.
4.3 Cultural Competence and Finding the Right Fit
The therapeutic relationship is profoundly personal. Finding a provider who understands your cultural background, race, ethnicity, religion, sexual orientation, or gender identity can be crucial for effective care. Many therapist directories now allow you to filter for these competencies. It is perfectly valid to seek out a provider who shares or has demonstrated expertise in your lived experience.
Conclusion: You Are the Captain of Your Journey
Navigating the U.S. healthcare system for mental wellness is undeniably difficult. The costs are high, the pathways are tangled, and the emotional toll is real. Yet, it is a navigable journey. By arming yourself with knowledge—of the system’s structure, its financial language, your legal rights, and practical step-by-step strategies—you reclaim a sense of agency.
The greatest cost is often the cost of inaction. The investment you make in your mental wellness, however arduous the process, pays dividends in every facet of your life: your relationships, your work, and your overall quality of life. You are worth the effort. Be persistent, be your own advocate, and remember that seeking help is not a sign of weakness, but one of profound strength and self-respect. The path to wellness exists, and you have the map.
Frequently Asked Questions (FAQ)
Q1: I think I need help, but I’m not sure if it’s “bad enough” for therapy. What should I do?
A: Therapy is not just for crises. It’s a tool for self-discovery, growth, and building coping skills for everyday challenges. If your thoughts or feelings are causing you distress or impacting your daily functioning, it’s “bad enough.” You do not need to be in crisis to deserve support. Many people benefit from therapy as a proactive, preventative measure.
Q2: What’s the difference between a psychologist, a psychiatrist, and a therapist?
A:
- Therapist/Counselor: This is a broad term for a licensed professional (LCSW, LPC, LMFT) who provides talk therapy.
- Psychologist: A doctoral-level professional (PhD or PsyD) who provides therapy and can conduct psychological testing. They generally cannot prescribe medication.
- Psychiatrist: A medical doctor (MD or DO) who can diagnose mental health conditions, prescribe and manage medication, and may also provide therapy.
A common care model is to see a therapist for weekly talk therapy and a psychiatrist (or sometimes a PCP) for medication management.
Q3: My insurance is denying claims for my therapy. What can I do?
A: This is frustrating but common. Your steps are:
- Call your insurance company and ask for a clear, detailed explanation of the denial.
- File an Appeal. All insurers have a formal appeals process. Your provider can often help by writing a letter of medical necessity.
- File a Complaint with Your State Insurance Department. If the internal appeal is denied, your state’s regulatory body can investigate, especially for potential parity law violations.
- Contact a Patient Advocate. Organizations like the Patient Advocate Foundation can provide free support and guidance.
Q4: Are online therapy platforms as effective as in-person therapy?
A: Research indicates that for many common conditions like depression and anxiety, telehealth can be just as effective as in-person care. The key factor for success is the quality of the therapeutic alliance, not the medium. However, it may not be suitable for severe, complex, or crisis-level conditions. It’s a personal choice based on your needs, preferences, and access.
Q5: How can I support a loved one who is struggling but refusing to get help?
A: This is one of the most challenging situations. Focus on:
- Expressing Concern, Not Judgment: Use “I” statements. “I’ve noticed you seem down lately, and I’m worried about you.”
- Listening Without Trying to “Fix”: Often, the person needs to feel heard and validated before they can consider action.
- Normalizing and Reducing Stigma: “It’s okay to not be okay. Many people see a therapist, it’s a sign of strength.”
- Offering Practical Help: “Would you like me to look up some therapists for you? Or would you like me to go with you to a first appointment?”
You cannot force someone into care, but you can plant seeds, offer support, and set healthy boundaries for yourself.
Q6: What if I can’t afford therapy even with a sliding scale?
A: Do not give up. There are still options:
- Community Mental Health Centers (CMHCs): These are mandated to provide care regardless of ability to pay.
- Crisis Hotlines: While not a replacement for therapy, they provide immediate, free support. The 988 Suicide & Crisis Lifeline is available 24/7 for any kind of crisis.
- Support Groups: Organizations like NAMI (National Alliance on Mental Illness) and the DBSA (Depression and Bipolar Support Alliance) offer free, peer-led support groups, both in-person and online.
- Self-Help Resources: Evidence-based workbooks (e.g., on CBT or ACT) and reputable mental health apps (like Woebot or Sanvello) can provide tools and structure while you seek professional care.